
A person experiencing depression who is treated with medication alone may report short-term relief (months to years) from symptoms, but may ultimately be unable to sustain a sense of the person they want to be. They can feel additional shame at being unable to be "cured", and over time lose hope. Additionally, the underlying mechanism causing the unwanted symptoms can continue to evolve. The effects of this on other areas of life such as health, work, and sociability can also worsen.
Is this "you have a disease" model interpretation of the life experience of a person's symptoms of depression or anxiety, for example, accurate or even helpful? Kinderman writes in an article in Mad In America of this phenomena: "We must move away from the ‘disease-model’, which assumes that emotional distress is merely symptomatic of biological illness, and instead embrace a model of mental health and well-being that recognises our essential and shared humanity." (Kinderman, 2004.)
I couldn't agree more. He begins the same article with an assessment of the current state of mental health treatment.
The idea that our more distressing emotions can best be understood as symptoms of physical illnesses is a pervasive, seductive but harmful myth. It means that our present approach to helping vulnerable people in acute emotional distress is severely hampered by old-fashioned, inhumane and fundamentally unscientific ideas about the nature and origins of mental health problems. We need wholesale and radical change in how we understand mental health problems and in how we design and commission mental health services.
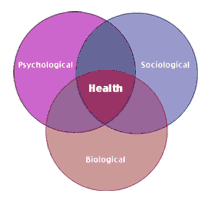
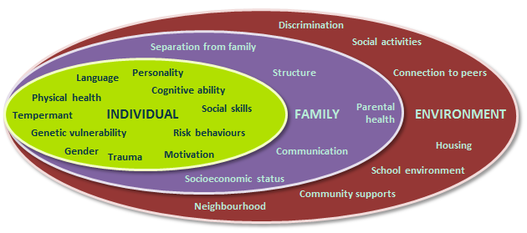
The apparent failure to take social factors into account "detracts from the idea that trauma in childhood is a very very powerful predictor of serious problems like experiencing psychotic events in adult life, so of course the brain is involved and of course genes are involved, but not very much, and an excessive focus on those issues takes us away from these very important social factors” says Kinderman in his radio interview.
For me, it's fascinating to watch members of the psychiatric profession learning that a person's history, including their social experiences are both symptom and cause in a dynamic and interactive way, determining and maintaining a useful or a not so useful way of being in the world.
Kinderman's belief that "services should be based on the premise that the origins of distress are largely social." (Kinderman 2014) is almost heretical. It represents a challenge to the dominant paradigm of medicalised mental health which, like most institutions, is conservative and slow to change. Indeed "Adopting this approach would result in a fundamental shift from a medical to a psychosocial focus." (Kinderman 2014) In other words, from automatically prescribing medication and medication alone, counselling and psychotherapy with a psychosocial understanding would become the dominant form of treatment.
In fact Narrative Therapy, developed in Australia by Michael White is already operating from that very premise. (White 1948-2008)
Narrative Therapy, by recognising the influence of society and an individuals position in that society, can significantly alter a diagnosis. Understanding that a cause is not biological or childhood trauma alone. A cause is often recognisably the result of how the experiences of that trauma have shaped how the person perceives themselves. Managing therapy with that in mind is radically different to any other form of therapy as it allows the individual to recognise themselves, themselves in relation to society, and in relation to institutions that inform that society by effectively externalising problems. You are not your problem; you are not your diagnosis. From that place, a meaningful understanding of self can occur, and a sustainable new narrative woven enabling a person to be in control again.
- http://www.madinamerica.com/2014/08/shh-just-whisper-might-just-revolution-underway/
- For publications relating to Narrative Therapy and to Michael White, refer to the Dulwich Centre.

 RSS Feed
RSS Feed